INTRODUCTION
Carotid-cavernous fistula (CCF) is a vascular disorder resulting from an abnormal connection between the carotid arteries and the cavernous sinus. In patients with CCF, arterial blood from the internal carotid artery or external carotid artery mixes with venous blood in the cavernous sinus. This results in increased pressure in the cavernous sinus and in the venous drainage vessels, along with a reversal of blood flow within them. Carotid-cavernous fistulas can be classified into various categories depending on their anatomy (direct and indirect fistulas), hemodynamics of blood flow (high- and low-flow fistulas), and etiology (traumatic, spontaneous) [1-4].
Direct CCFs are the most common type. They involve a direct connection between the internal carotid artery (ICA) and the cavernous sinus. Based on their hemodynamic characteristics, they are classified as high-flow fistulas. In the vast majority of cases, direct fistula results from trauma causing damage to the ICA wall. The ICA segment traversing through the cavernous sinus is particularly susceptible to trauma in cases of basilar skull fracture [5]. Carotid-cavernous fistula is estimated to affect 0.2% of patients following craniocerebral trauma [2] and 3.8% of patients with basilar skull fractures [6]. In their review of 91 cases of direct carotid-cavernous fistulas, Gupta et al. [7] found that trauma was the underlying cause in 85 cases, and aneurysm rupture in the remaining six cases. Direct CCFs may also, though very rarely, occur idiopathically, especially in patients with conditions predisposing them to disorders of muscle tissue and collagen fibers.
Indirect CCFs are less prevalent. Hemodynamically, they are low-flow fistulas, and they originate through indirect communication between the cavernous sinus and the ICA or ECA via their meningeal branches. The majority of indirect CCFs occur spontaneously; however, a link has been found between their incidence and hypertension, female gender, and older age [4, 5].
The clinical presentation varies depending on the fistula size and its hemodynamic characteristics. Direct CCFs have a rapid onset and severe manifestations. Patients present with the classic triad of symptoms including proptosis, orbital bruit, and conjunctival chemosis on the affected side. In indirect fistulas, where blood flow is slower, clinical symptoms tend to develop more slowly and are less pronounced [8].
Common manifestations of the disorder include impaired eye movement and ptosis (caused by damage to the cranial nerves III, IV, and VI). The symptoms arise from the anatomical pathways of these nerves within the cavernous sinus. Patients may also present with visual field loss and facial pain in the region innervated by the first and second branches of the trigeminal nerve. Prolonged disease duration may lead to elevated IOP with secondary glaucoma, central retinal vein thrombosis, and intravitreal hemorrhage. The observed IOP increase is attributed to retrograde blood flow from the cavernous sinus into the superior ophthalmic vein, leading to elevated pressure in the episcleral veins and hindered outflow through the Schlemm’s canal [9, 10].
CASE REPORT
A 78-year-old female patient reported to the emergency room of the Ophthalmology Department at Prof. K. Gibiński University Clinical Center, Medical University of Silesia in Katowice, Poland, because of a decline in visual acuity in her right eye persisting for approximately two months. The family members stated that the patient had also exhibited redness of the eyelids in the RE for the past two weeks and proptosis of the RE for the past two or three months. Both the patient and her family denied any history of accident or injury. The patient had been treated for dementia but she had not received any prior ophthalmic treatment.
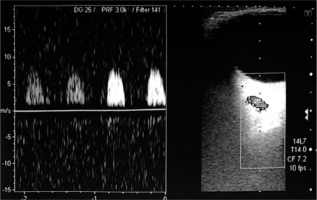
Ophthalmological assessment revealed best corrected visual acuity of 0.1 in the right eye and 0.6 in the left eye, as determined by the Snellen test. The intraocular pressure measured by Goldman applanation tonometry was 27 mmHg and 17 mmHg in the right and left eyes, respectively. Clinical examination revealed proptosis in the RE, slightly limited RE motility in all directions, venous congestion, chemosis of the bulbar and palpebral conjunctiva in the RE, and bilateral corticonuclear cataract (Figure 1). The cornea of the RE exhibited signs of exposure keratopathy, with visible tear film loss (TBUT test < 5 s). Examination of the posterior segment of the RE revealed isolated diffuse retinal petechiae and a flat peripheral choroidal detachment. No abnormalities were seen in the posterior segment of the left eye. Ocular ultrasound showed a flat choroidal detachment, extending up to 7 mm, in the posterior pole of the right eye (Figure 2).
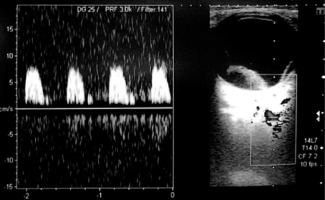
The patient was admitted to the Ophthalmology Department for an extended diagnostic assessment and inpatient treatment. Treatment with topical IOP-lowering agents (timolol, brinzolamide) was initiated, along with topical lubricants (Carbomer 980 – 2 mg/g, 2.0% trehalose, and 0.25% sodium hyaluronate) to prevent exposure keratopathy. A general blood panel was ordered, including thyroid hormone level and TRAb antibody tests. Ultrasound examination of the RE was repeated, revealing a hypoechoic structure in the retrobulbar location. The diagnostic workup was extended to include Doppler ultrasound, which demonstrated marked dilatation of the superior orbital vein with arterialized blood flow in the lumen (Figures 3 and 4). Static perimetry revealed significant narrowing of concentric visual field in both eyes, and absolute and relative scotomas, more severe in the RE (Figures 5 and 6).
Optical coherence tomography (OCT) revealed significant bilateral thinning of the retinal ganglion cell complex, along with defects in the retinal nerve fiber layer (RNFL). Orbital magnetic resonance imaging showed thickening and swelling of the extraocular muscles of the RE, inflammatory changes within the soft tissues of the right orbit with extensive detachment of the retinochoroidal complex, and right-sided dilatation of the superior ophthalmic vein, up to 3 mm.
Based on the clinical presentation and additional examinations, a suspicion of a right-sided carotid-cavernous fistula was raised.
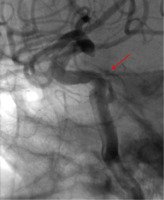
Following the treatment, there was a slight reduction in the patient’s local symptoms, and the IOP in the RE had returned to normal. The patient was transferred to the Department of Neurosurgery for digital subtractive angiography (DSA), which showed a direct carotid-cavernous fistula accompanied by moderate secondary venous dilatation in the right orbit (Figure 7).
Due to deterioration of visual acuity in the RE, secondary glaucoma, and the patient’s subjective symptoms, the decision was made to proceed with fistula embolization. The procedure was performed in the Neurosurgery Department, in a standard manner, without complications. Partial embolization of the fistula was achieved (Figure 8).
During the patient’s postoperative follow-up, her general condition deteriorated. Magnetic resonance imaging of the head was performed, demonstrating embolization material in the right middle cerebral artery. In addition, ischemic changes were detected within the head of the right caudate nucleus, in the anterior portions of the external and internal capsules, and in the anterior lenticular nucleus. The patient received a neurological consultation, which confirmed a correlation between the CNS lesions enumerated above and the symptoms presented by the patient. Anticoagulant therapy was initiated, and the patient’s arterial blood pressure was closely monitored. After a 10-day hospital stay, the patient was discharged home.
A follow-up examination at the ophthalmology outpatient clinic, conducted one month after embolization, revealed best-corrected distance visual acuity of 0.6, and the IOP of 16 mmHg in both eyes. Examination of the anterior segment of the eye showed dilated tortuous scleral vessels, and corticonuclear cataract with no signs of progression. No proptosis was observed in the RE, and ocular motility was full in all directions. Mild signs of exposure keratopathy were observed (Figure 9). However, based on reports from the patient’s family, there was a notable decline in her cognitive abilities, and she required third-party assistance in daily activities.
DISCUSSION
In the reported case, the patient’s carotid-cavernous fistula was associated with ophthalmic complications that could potentially result in permanent damage to the organ of vision. Based on additional examinations, secondary glaucoma was diagnosed; however, due to the absence of prior ophthalmic assessments, it is difficult to definitively ascertain whether the fistula was the sole pathomechanism responsible for the damage to the ganglion cell complex and optic nerve fibers.
The treatment of CCFs depends on the severity of clinical symptoms, the type of fistula, and the associated risk of intracranial hemorrhage [11]. According to the literature, direct high-flow fistulas require treatment because they carry a high risk of intracranial bleeding. Low-flow indirect CCFs, whether asymptomatic, incidentally detected, or minimally symptomatic, are not normally associated with a significant risk of intracerebral hemorrhage. In such cases, ophthalmic symptoms are typically managed conservatively using local medications or external pressure on the carotid artery (6-15 times a day for 10 seconds) [12, 13]. If the symptoms result in chronic ophthalmic complications, endovascular interventions are recommended. The first-line therapeutic option should be endovascular embolization with balloons, coils, stents, or liquid embolic agents. The procedure can be conducted from either an arterial or venous approach, with a high rate of successful outcomes [14, 15]. Where embolization is not a suitable modality or it proves ineffective, surgical options such as ligation of the internal carotid artery or cavernous sinus packing should be recommended. Stereotactic radiosurgery may be considered as an alternative therapy for low-flow CCFs, but it does not play a prominent role in the treatment of high-flow CCFs [16].
When deciding on the surgical treatment of a carotid-cavernous fistula, it is important to weigh the risk of intra- and postoperative complications, especially the potential for embolism of blood vessels in the CNS, which could result in permanent adverse neurological effects [17-19].
CONCLUSIONS
A direct carotid-cavernous fistula with accompanying symptoms and ophthalmic complications threatening vision loss requires interventional radiological treatment. However, it needs to be noted that even with the resolution of ophthalmic symptoms and partial embolization of the fistula, adverse postoperative outcomes (such as secondary CNS stroke) may still occur, as in our reported patient.
The patient requires ongoing neurological and ophthalmological care. The embolization procedure was successful, and the ocular symptoms of CCF did not recur during the six-month follow-up period.

 ENGLISH
ENGLISH