INTRODUCTION
Recent years have brought great advances in ophthalmology, specifically in ophthalmic surgery. This rapid development is connected with the development of technology, including many innovations in surgical tools and machines, as well as intraocular lenses.
Worldwide, cataract surgery is one of the most frequently performed operations in ophthalmology, the gold standard being small incision phacoemulsification with intracapsular implantation of the intraocular lens (IOL). Cataract surgery with artificial IOL implantation is the most frequently performed type of surgery in the European Union (EU) – Eurostat data confirm 4.2 million procedures in the EU countries in 2015 alone [1].
The purpose of contemporary cataract surgery is not only to remove the opaque lens, but also to achieve the best possible uncorrected and best-corrected visual acuity. Ideally, postoperatively, the patient should have full visual acuity for distance, without the need of spectacle correction. Astigmatism is one of the factors limiting both the refractive and functional results of phacoemulsification.
In eyes undergoing phacoemulsification, a standard monofocal intraocular lens does not correct preoperative astigmatism; therefore, patients still require optical correction for distance after the surgery.
Many modern types of intraocular lenses have been introduced in recent years, including blue light blocking lenses, multifocal lenses, accommodating lenses, light adjustable lenses, and astigmatism-correcting toric lenses. They all address specific needs and they allow better functional results to be achieved after cataract removal.
Toric intraocular lenses are indicated for patients with clinically significant corneal astigmatism, who want to reduce the cylindrical component of their refraction. After phacoemulsification with a toric intraocular lens implantation, patients require only spherical correction for near vision, as the need to correct astigmatism with cylinders is eliminated.
In order to preserve the optical properties of the toric lens, it is necessary to properly place it in the capsule during the surgery (in the right axis). Moreover, the lens must remain stable in the same position in the postoperative period, as any spontaneous rotation reduces its optical performance.
AIM OF THE STUDY
The aim of the study was to evaluate and compare functional results of phacoemulsification with intraocular toric lens implantation, as well as to compare the spontaneous rotation of two models of toric intraocular lenses in patients with preoperative corneal astigmatism.
MATERIAL AND METHODS
In this prospective observational study two groups of patients were evaluated after planned standard phacoemulsification surgery with implantation of a foldable, acrylic toric IOL.
After being explained the details of the study, patients gave informed consent and were randomly assigned to one of the groups. All procedures were performed in the Department of Ophthalmology, Medical University of Lodz, Poland.
For all study protocols all tenets of the Declaration of Helsinki were followed. The study was approved by the Bioethics Committee of the Medical University of Lodz, Poland (no. RNN/230/13/KE).
Inclusion and exclusion criteria
Patients who fulfilled the following inclusion criteria were included in the study: the existence of cataract which qualified for cataract surgery and lack of any exclusion criteria.
Exclusion criteria included: amblyopia, congenital ocular malformations, any previous ocular surgery, previous ocular trauma, corneal disorders, preoperative corneal endothelial cell density lower than 1500 cells/mm2, retinal and macular disorders, history of uveitis, glaucoma, diabetic retinopathy, connective tissue diseases, complicated phacoemulsification surgery and presence of any other diseases that could affect the postoperative outcomes.
All patients had a similar degree of nuclear (NO2 or NO3) and cortical opacification (C2 or C3) assessed according to the LOCS III scale.
Patients who fulfilled the inclusion criteria and consented to participate were randomly assigned to one of the groups.
Surgical technique
All patients underwent the same type of phacoemulsification, but received different intraocular lenses.
In all patients, before the surgery topical tropicamide 1% (Tropicamidum WZF 1%) and phenylephrine hydrochloride 10% (Neosynephrin-POS 10%) were used to dilate the pupils.
All surgical procedures were performed under topical anaesthesia, namely: proxymetacaine hydrochloride 0.5% eyedrops (Alcaine), topically administered 2% lidocaine gel and 1% lidocaine solution administered intracamerally. In all patients the pupil was dilated before the surgery with a 1% solution of tropicamide and phenylephrine (NeoSynephrine).
All phacoemulsifications were performed using a Centurion phaco machine (Alcon). In all eyes the same surgical settings of the machine were used, and the same ophthalmic viscosurgical device (OVD) (hydroxypropyl methylcellulose 2.0% in saline solution [EYEFILL H.D., Bausch & Lomb]) and the same infusion fluid (BSS – balanced salt solution) were used.
First, a self-sealing 2.4 mm clear corneal incision was created temporally with a 2.4 mm knife (MSL 24, Mani). Two side ports (paracenteses) were created with an MVR 20G knife, 90° away from the main incision. After continuous curvilinear capsulorhexis was created with microforceps, hydrodissection was performed. Next, phacoemulsification and irrigation-aspiration were performed. A one-piece intraocular lens was implanted in-the-bag through the main 2.4 mm incision with an injector. The toric lenses had orientation marks; the axis of rotation was determined from a line bisecting the IOL orientation marks.
In all patients, at the end of the surgery, saline solution (0.9% NaCl) was used for the stromal hydration of the corneal wound.
No additional astigmatic correction (e.g. arcuate incisions) was used at the time of the surgery. Postoperative management was the same in all patients and included a topical combination of tobramycin-dexamethasone (Tobradex) eyedrops 4 times daily for 3 weeks after the surgery.
Group 1 included patients with preoperative corneal astigmatism above 1.5 diopters (D) who underwent implantation of an Acrysof IQ Toric lens (Alcon, USA). This group consisted of 27 eyes of 27 patients (21 women [78%] and 6 men [22%], aged from 40 to 86 years [mean age 65 ±14 years]). Mean preoperative corneal astigmatism was 3.6 ±1.0 Dcyl. Mean lens opacity according to the LOCS III scale was 2.63 ±1.0.
Group 2 included patients with preoperative corneal astigmatism above 1.5 diopters who underwent implantation of a Tecnis Toric lens (AMO, USA). This group consisted of 23 eyes of 23 patients (16 women [70%] and 7 men [30%], aged from 38 to 83 years old [mean age 67 ±11 years]). Mean preoperative corneal astigmatism was 2.75±1.0 Dcyl. Mean lens opacity according to the LOCS III scale was 2.64 ±1.0.
Patient examinations
In all patients preoperative biometry was performed using the IOL Master optical biometry device (version 5.4). The IOL calculation formulas were in accordance with the Royal College of Ophthalmologists (UK) guidelines 2004: for eyes with axial length below 22.0 mm the Hoffer Q formula was used, while for axial lengths equal to or greater than 22.0 mm the SRK/T formula was applied.
Patients were examined before the surgery, as well as 1 day and 1 month after the surgery. All examinations and measurements were performed by one doctor (SF).
In all patients the following examinations were performed at each visit: best corrected distance visual acuity (BCDVA) using standard Snellen charts, evaluation of the anterior and posterior segment using a biomicroscope, autorefractometry with a Tomey autorefractometer (RC-5000), tonometry, keratometry and anterior segment photography after dilating the pupil.
Before the surgery, the two ends of vertical and horizontal planes were determined and marked on the corneal limbus using a sterile manual corneal marker with an in-built level, which was inked just before the marking was done. The vertical and horizontal planes were marked with the patient sitting at the slit lamp and looking at a distant target with the fellow eye. In the second step, during the surgery, the astigmatic axis was marked using a new sterile inked marker with a caliper, which was rotated according to the axis determined by the biometry.
ToriCalc software
Based on the anterior segment photography the toric lens rotation was calculated with purpose-designed software called ToriCalc. The software was custom designed by Dr Michal Wilczynski and it was written (coded) by Maksym Mikołajczyk.
The software allows one to load two photos for comparison. It was designed to use slit-lamp photos, but any photos could be used.
First, after appropriate pupil dilation, the patient was positioned at the slit-lamp and the head position was adjusted in order to avoid any error resulting from head tilt. Retroillumination was used for better IOL visualization. Next, a photograph was taken using an in-built slit lamp camera, or alternatively, using a camera-enabled mobile phone mounted to a slit lamp.
Then the custom-built ToriCalc software was used to analyze the image.
After entering the patient’s data (which is optional), in the first step, the user can adjust the relative rotation of photos, in order to eliminate the influence of the patient’s head tilt. The user can indicate two characteristic points in the photo (e.g. conjunctival vessel crossings or bifurcations) in both photographs, and the software draws a line between the two chosen marking points and adjusts the rotation of the second photo according to the markings in the first photo.
Next, two points are placed on the IOL marking dots on opposite sides of the optic and a line is drawn between the dots. The cosine theorem is used to measure the angle between the two lines. The result is the toric IOL rotation. The ToriCalc software did not store any data, which were removed from computer memory after the program was closed.
To provide high accuracy of measurement, the user can zoom in on the photo and adjust its position, allowing the angle-determining points to be placed exactly on the IOL marking dots.
Furthermore, when the angle is obtained, a representation of the lens rotation can be shown on a Cartesian coordinate system graph. Such a depiction is a clear way to represent the data visually and can also prove useful when explaining the situation to the patient.
Finally, a report can be printed or saved to the hard drive in a common document format (PDF). The report consists of the patient’s data (if supplied), both photos with applied user-side transformation of adjusted rotation, position and scale, with the lines used to determine the angle of toric IOL rotation. Additionally, numeric data regarding the angles are also supplied. If generated, the representational graph is the final element of the report. Figure 1 shows an example printout from the ToriCalc software.
Description of mathematical functions
The key feature of the application is the calculation of toric IOL rotation difference in a given time period from two photos. To perform this task, the cosine theorem for two vectors of known direction and value is applied. Before the derivation of the final equation used for measurement, it is worth recalling how to calculate the length of a vector and the dot product function. The length of a vector is the square root of the sum of its coordinates squared [1]. It can be derived straight from the Pythagorean theorem. In short, the dot product is an algebraic operation, which allows a scalar result to be acquired by multiplying two vectors [2]. The length of a vector and dot product can be combined by squaring the length of the vector. Instead of multiplying a given number by itself, we get the dot product [2]. The information provided above is crucial for understanding how to transform the cosine theorem to acquire a function, which allows calculation of the angle between two vectors [3]. Supplying data from the graph to the equation, we receive a short inverse cosine function from the quotient, where the numerator is the dot product of two vectors and the denominator is the product of their lengths.
The code was written in Java script language, used in the web version of the application. However, the function has a drawback – the direction of rotation is not known. Thus, in our application the vector created by the lens rotation is compared to a horizontal vector (OX axis). This way we obtain the toric IOL angles on both photos, from which we can take the difference (knowing that a negative result is counterclockwise rotation).
The next step was vector determination. The width of the photo was used as the X axis and the height as the Y axis, thus creating a simple Cartesian coordinate system between zero and width and zero and height. By clicking on the photo, the user adds points, between which a line segment is drawn. To acquire vector coordinates, one point’s coordinates are subtracted from the other point’s coordinates. For coherence, the application chooses the point with a lower Y value as the start of the vector.
Next, using the function derived above, the difference of angles is calculated. The graphical user interface was written in HTML with CSS – a standard in web development. The logic was supplied by JavaScript language, interpreted directly in the user’s browser [5]. After loading images, the user can adjust the rotation of the images to account for patient head tilt. The rotation is performed by supplying matching points on both photos (e.g. conjunctival vessel crossings or bifurcations), and matching the vector rotations so that the second photo has the same angle as the first. To increase measurement precision, the user can also move and scale created points.
The last step before printing the report is an option to generate an interactive graph, depicting both rotations on a Cartesian coordinate circle.
Statistical methods
Non-parametric tests were used for statistical analyses. Pre- and postoperative values in the same group (dependent samples) were compared using the Wilcoxon signed-rank test. Statistical significance of differences between unpaired data (independent samples) was determined using the Mann-Whitney U test. All calculations were performed for the significance level α = 0.05. Differences were considered statistically significant at p < 0.05.
RESULTS
All procedures were uneventful. We did not observe corneal burns or any other complications.
Best corrected distance visual acuity (BCDVA)
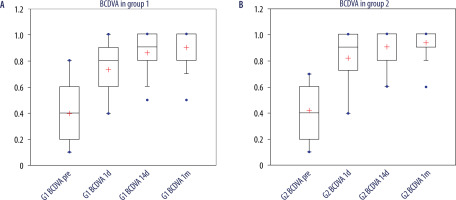
In the current study, there were no statistically significant between-group differences in mean BCDVA preoperatively and throughout follow-up after surgery (Figure 2). Preoperative BCDVA was 0.40 ±0.24 in group 1 and 0.42 ±0.20 in group 2. The difference between the groups was not significant (p > 0.05). In both groups a postoperative gradual and significant increase in BCDVA was observed. One month after the surgery it was 0.90 ±0.13 in group 1 and 0.94 ±0.1 in group 2. The difference between the groups was not significant (p > 0.05).
Uncorrected distance visual acuity (UCDVA)
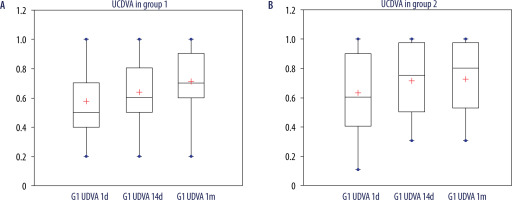
In both groups a postoperative gradual and significant increase in UCDVA was observed (Figure 3). One month after the surgery it was 0.71 ±0.23 in group 1 and 0.72 ±0.24 in group 2. The difference between the groups was not significant (p > 0.05).
IOL rotation
Mean spontaneous IOL rotation in group 1 was 0.75 degrees after 14 days; later this value increased to 0.81 after 30 days. Similarly, mean spontaneous IOL rotation in group 2 was 0.81 degrees after 14 days; later this value increased to 0.91 after 30 days. The rotation of the toric IOL was not significant in both groups. Moreover, the difference in the mean IOL rotation between the groups was not significant (p > 0.05).
Residual refractive error (spherical component)
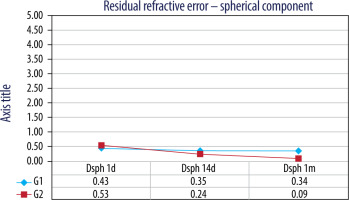
We found that the spherical component of the residual refractive error, measured by autorefractometry, was significantly lower after the surgery compared to preoperative values (p < 0.05) (Figure 4). Nevertheless, no significant difference between the groups was found (p > 0.05).
Residual refractive error (cylindrical component)
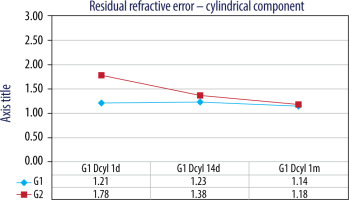
We found that the cylindrical component of the residual refractive error, measured by autorefractometry, was significantly lower after the surgery compared to preoperative values (p < 0.05) (Figure 5). Nevertheless, no significant difference between the groups was found (p > 0.05).
DISCUSSION
With continuous development of technology and evolving patients’ expectations of outcomes, an increasing number of patients expect spectacle independence after cataract surgery.
It is estimated that almost 60% of cataract patients have at least 0.75 D of corneal astigmatism [2]. Preoperative astigmatism is an important factor which limits the possibility of achieving full uncorrected visual acuity. For this reason, many treatment modalities have been introduced.
There are many methods of surgical correction of astigmatism, including limbal relaxing incisions (LRIs), two opposite clear corneal incisions, keratotomy, toric intraocular lenses, as well as various laser refractive surgery techniques.
While performing cataract surgery, it is possible to use stable and controlled correction of preoperative astigmatism. Implantation of a toric intraocular lens is one of the most frequently used methods of correcting preoperative astigmatism [3]. The introduction of various models of toric intraocular lenses has allowed the problem of preoperative corneal astigmatism to be solved. In recent years, toric intraocular lenses have become more popular in the treatment of preoperative astigmatism. In order to maintain optical properties of the toric lens, both its precise intraoperative positioning and its stable position in the postoperative period are necessary.
Preoperatively, both the power and the target position of the toric IOL are calculated for each eye individually, usually using an online calculator offered by the IOL manufacturer. At the beginning of the surgery, precise axis marking on the eyeball is necessary. Various methods are used for this purpose – from a simple pen marker to very complex electronic systems in-built in the operating microscope.
It is known that in the postoperative period, the IOL may rotate. In the case of toric IOLs, this phenomenon has great importance as it can significantly reduce the effectiveness of the astigmatic correction [4, 5].
Several factors influence the proper position of the toric IOL, including the following: precise preoperative calculation of the power and angle of the cylinder, precise preoperative axis marking, thorough IOL positioning during implantation, the type of implanted IOL, thorough aspiration of the viscoelastic (OVD) from the capsule during the surgery, as well as spontaneous postoperative rotation.
The rotational stability of the intraocular lens in the postoperative period directly influences the refractive result of the procedure. In some studies it was found that postoperatively toric lenses may rotate as much as 30 degrees and that each 3 degrees of rotation diminishes the cylindrical correction by 10%, which means that rotation of 30 degrees (which corresponds to 1 clock hour) reduces effective astigmatic correction to zero [5]. For this reason, it is important to evaluate the rotational stability of various models of toric lenses.
Measurement of postoperative IOL alignment is crucial to determine whether the IOL is properly positioned, whether any decrease of visual acuity results from the changed IOL position and whether the IOL is rotationally stable.
There is no single universal method for monitoring and evaluating the postoperative rotation of the IOL. Various methods of measuring postoperative IOL rotation are known, the most popular being a slit-lamp examination with measurement of the angle of the slit. The examiner dilates the patient’s pupil and rotates the slit so it is superimposed on the toric markings of the IOL. The main disadvantage of this technique is the fact that it is possible to improperly align the slit with IOL markings, which can make the measurement imprecise. Moreover, uneasy patients who move their eyeball during the slit adjustment also may compromise the precision of the measurements. Moreover, a few methods using a mobile phone camera or slit lamp photography have been described [6-9]. Therefore, a simple, repeatable and precise method of measuring toric intraocular lens rotation would be useful.
We present a simple technique for measuring postoperative toric IOL rotation using slit-lamp photos and custom-built software which takes into account both relative rotation of consecutive photographs and rotation of the toric IOL axis. The software-guided evaluation has many benefits – it is quick, easy, precise and usually allows the data to be either stored or printed.
The presented technique for measuring postoperative toric IOL rotation using slit-lamp photos and a custom-built software is simple and the software takes into account and corrects relative rotation of consecutive photographs, resulting from patients’ head tilt. This feature increases the precision of measurements. An additional advantage is the possibility to print a report in order to save it in the medical records for archiving purposes.
In our study we found that both evaluated IOLs offer excellent and similar rotational stability and very good functional results.
CONCLUSIONS
Based on the study and the analysis of the results, we found that both the examined IOLs, namely the Acrysof IQ Toric lens (Alcon, USA) and the Tecnis Toric lens (AMO, USA), offer excellent and similar rotational stability and very good functional results. There was no significant difference between the results obtained with these two toric IOLs.
The software-guided postoperative evaluation of rotational stability of implanted toric intraocular lenses is a good method of evaluating the position of IOLs, which enables precise measurements.

 ENGLISH
ENGLISH